Epidural blood patch
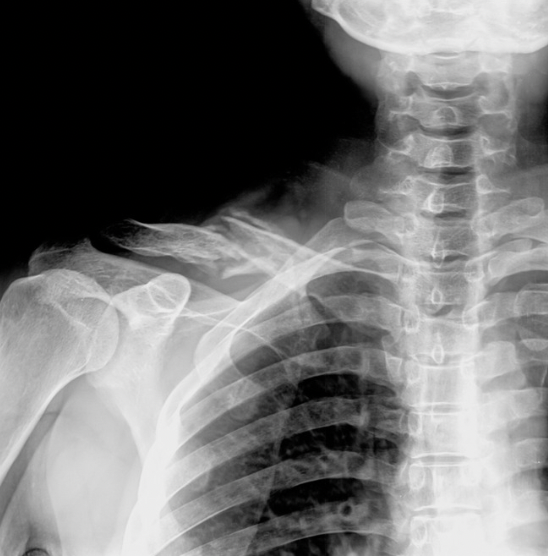
Epidural blood patch (EBP) is a well-established procedure for treatment of cerebrospinal fluid (CSF) leaks arising from the spinal column. It uses autologous blood (the patient's own blood) injected into the epidural space. The spinal cord is enclosed within a sac of CSF, which is contained by a membranous later called the dural sac. The epidural space is the space between this dural sac and the bony vertebral column. The blood injected is thought to clot and therefore effectively 'patch' the hole in the dura.
What condition does it treat?
EBP is routinely used to relieve post dural puncture headaches caused by epidural contractions, but it is important to note that CSF can can have other causes. For example, spontaneous or traumatic causes such as fall or whiplash injury. The tear/hole in the dura can cause CSF to leak out which can lower CSF pressure and lead to postural headaches, neck pain and other neurological symptoms. Such headaches are worsened when sitting upright and relieved when laying down. Widespread pain and inflammation is also possible.
CSF leaks can be difficult to diagnose as symptoms vary between patients, hence a patient's response to EBP can also be used to confirm the diagnosis.
How is it Performed?
EBP is performed under sterile conditions in an operating theatre using mild sedation. Fluoroscopic x-ray guidance is used to ensure precision and accuracy when positioning the epidural needle. A doctor will access a vein via a cannula in the arm for drawing blood and maintaining sterilisation. Gradually, variable amounts of blood will be injected into the epidural space.
You may be asked for feedback about the procedure regarding pressure levels/response. EBP is typically performed laying on your stomach. Your blood pressure and oxygen rates will be monitored.
How do i prepare for the procedure?
Avoid eating or drinking for 6 hours prior
Consult with your doctor in advance if you are taking diabetic or blood thinning medications
when to call your doctor or nurses at mpg?
Contact your doctor or nurse if you have increasing pain after 24 hours, signs of infection (eg. fever or chills), new onset limb weakness, numbness, trouble emptying bladder and/or bowels, a stiff neck, photophobia (aversion to bright light), severe headache or increased or severe head pressure behind the eyes which is worsened with lying down.
Side effects & complications
General sedation/procedural risks: drowsiness, infection, local damage to structure, headache
Transient back pain - pain may last up to 4 weeks
Transient radicular pain - pain down leg/s
Local swelling
General sedation/procedural risks: drowsiness, infection headache
A feeling of increased pressure in your head as blood volume is injected (transient). It is important to note that this transient increase in pressure is a normal feature and a sign that the procedure is being executed effectively
What to expect after the procedure
You will be taken to the recovery room for a few hours to lay down and monitor pain levels, blood pressure and vital signs. Your treating doctor will discuss laying on your back for 4-6 hours. Preferably, you will be kept overnight, and must be driven home by a carer post-procedure. Once home, it is advised to lie down and rest for the next 24-48 hours. Light activity may be resumed the next day. Returning to work may take longer depending on individual circumstances and previous function levels.
Post ebp care and restrictions
Avoid anti-inflammatory medications - up to 7 days, check with your doctor
Log roll to get into/out of bed, meaning maintaining a straight spine. Your physiotherapist or nurse will demonstrate - 2-4 weeks
Avoid twisting, bending, stretching, or lifting anything heavier than 2-3kg - 6 weeks
Avoid straining. Do not hold your breath or strain on the toilet (use laxatives if required)
Try not to sneeze - if you must, try to keep your mouth open - 6 weeks
Do not bend forwards to lift things off the floor - 6 weeks
If you do need to lift, bend your knees, keep back straight, do not hold your breath
Limit driving/sitting time for 1 week. Recline back seat if you are a passenger
Commence a daily walking program after 2-3 days. Keep a walking diary and aim to gradually increase distance on flat terrain - 6 weeks
Resume strenuous activity such as sports 6 weeks to 3 months depending on discussions with your treating team
Diet: maintain fluids with electrolytes. Avoid foods high in vitamins, limit salt and avoid caffeine, as these can increase rebound pressure.
Rebound intracranial hypertension: Only occurs in roughly 33% of causes, but is more common in chronic, long term CSF leaks. Symptoms include a severe pressure headache in the forehead or behind the eyes, tinnitus (ringing/pulsing in the ears) and increased head pain when lying down, eg. a change in headache pattern.
Note: if you do have rebound high pressure symptoms, treatment may include simple lifestyle and diet advice or certain medications may be advised - discuss with you doctor.
Key management points to know
The timeframe to notice whether improvement has occurred as a result of EBP may vary between patients. You may notice immediate improvement within 24-48 hours or it may take 1-2 weeks of gradual ability to maintain upright posture for a longer duration.
A positive response can be used as a diagnostic took and symptom relief may or may not be sustained
Multi-level or targeted EBP's are a variation to discuss with your treating physician
The success rate of non-targeted epidural blood patch is variable, reported between 50-95% for craniospinal hypotension and 90-99% for post lumbar puncture headache and sometimes multiple EBP's are required for a successful outcome
Rescheduling and enquiries
Should you have any enquiries or require rescheduling of your procedure, please notify the Clinical Support Team on 03 8548 0339.